Publication Detail
Detection of SARS-associated coronavirus in throat wash and saliva in early diagnosis.
Wang WK, Chen SY, Liu IJ, Chen YC, Chen HL, Yang CF, Chen PJ, Yeh SH, Kao CL, Huang LM, Hsueh PR, Wang JT, Sheng WH, Fang CT, Hung CC, Hsieh SM, Su CP, Chiang WC, Yang JY, Lin JH, Hsieh SC, Hu HP, Chiang YP, Wang JT, Yang PC, Chang SC.
Citation
Wang WK, Chen SY, Liu IJ, Chen YC, Chen HL, Yang CF, Chen PJ, Yeh SH, Kao CL, Huang LM, Hsueh PR, Wang JT, Sheng WH, Fang CT, Hung CC, Hsieh SM, Su CP, Chiang WC, Yang JY, Lin JH, Hsieh SC, Hu HP, Chiang YP, Wang JT, Yang PC, Chang SC. (2004) Detection of SARS-associated coronavirus in throat wash and saliva in early diagnosis. Emerging Infectious Diseases 10(7):1213-1219.
Abstract
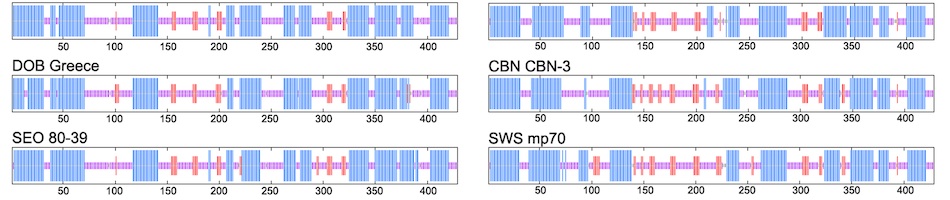
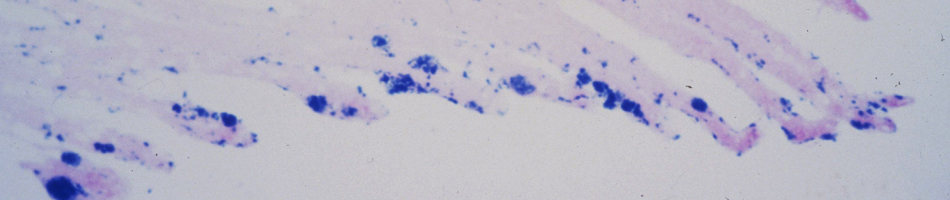
The severe acute respiratory syndrome-associated coronavirus (SARS-CoV) is thought to be transmitted primarily through dispersal of droplets, but little is known about the load of SARS-CoV in oral droplets. We examined oral specimens, including throat wash and saliva, and found large amounts of SARS-CoV RNA in both throat wash (9.58 x 10(2) to 5.93 x 10(6) copies/mL) and saliva (7.08 x 10(3) to 6.38 x 10(8) copies/mL) from all specimens of 17 consecutive probable SARS case-patients, supporting the possibility of transmission through oral droplets. Immunofluorescence study showed replication of SARS-CoV in the cells derived from throat wash, demonstrating the possibility of developing a convenient antigen detection assay. This finding, with the high detection rate a median of 4 days after disease onset and before the development of lung lesions in four patients, suggests that throat wash and saliva should be included in sample collection guidelines for SARS diagnosis.
| Link: | http://www.ncbi.nlm.nih.gov/pubmed/15324540 |
| PMID: | 15324540 |
| PMCID: |